Starting in the mid-1930s three types of shock therapies began to be introduced to the DCMH. The first one was Cardizol Shock Therapy in 1934. The origins of this treatment date back to the serendipitous observation that people suffering from a combination of epilepsy and psychosis became lucid during fits (Kennedy, 1937). It was subsequently deduced that seizures might cure psychoses (McCrae, 2006). Based on these ideas, the Hungarian Ladislas von Meduna introduced shock by Cardiazol, a camphor-like substance which would be injected. The treatment was hazardous with patients suffering joint dislocations, spinal hairline fractures and even dying from ‘status epilepticus’ – on top of this, conclusive scientific evidence that the treatment actually worked was lacking. The Medical Superintendent, however, stated in his 1941 annual report somewhat prematurely and over-enthusiastically that the ‘value [of Cardiazol shock] is beyond doubt’ (Medical Superintendent’s Annual Report, 1941). Similar success was reported to patients’ relatives who had frequently consented to the patient’s treatment ‘[…] we too are pleased with the result of the injection treatment and the patient’s condition is so much better that we feel she might go home soon’ (Correspondence regarding ER). Unfortunately, for the patients ‘recovery’ was usually short-lived and many a patient slipped back into their previous depressed condition only to receive more injections. Despite the risks involved, relatives readily agreed to patients being injected with Cardiazol and while this seems disturbing from today’s perspective, it must be acknowledged that making an informed decision was at that time not only made difficult owing to limited information on the consent forms, but some grossly understated the risks involved in the treatment. A consent form for Cardiazol treatment handed out in the late 1930s, for example, states that ‘the risk from this form of treatment (Cardiazol therapy) is slight’. It does, however, mention that the treatment will be applied ‘as the patient is not re-acting [sic] satisfactorily to the usual methods of treatment’, suggesting Cardiazol therapy was a last resort. On other occasions it was not evident from the form to which kind of therapy the relative was consenting. A form used in the early 1940s, for example, reads ‘I shall be glad if you give your consent to commence a course of Electrical or Cardiazol therapy in the case of the above named’.
In June 1937 another form of shock treatment was first practised in the DCMH. Insulin Coma Therapy (ICT) had been developed by the Austrian Manfred Joshua Sakel two years before. Here, patients received injections of insulin, starting with 20 units at 7am. The number of units given each morning was incrementally increased ‘until sweating occur[red]’ – in several cases up to 440 units, and some patients endured as many as 51 comas.
This form of treatment was extremely labour-intensive, as the patients’ vital signs had to be constantly monitored because irreversible coma resulting in the patient’s death was only one of the possible complications. A vivid account of the unpleasantness of this treatment can be found in Wilson (1936). Once woken up, the patients were fed sweetened tea and glucose to restore the bodily balance. As with many of the other early physical treatments, the efficacy of ICT was scientifically unproven and soon refuted (Bourne, 1953; Acker, Harris & Oldham, 1957), but in the DCMH it was found to be of particular benefit for patients suffering from schizophrenia – although the Medical Superintendent lamented that ‘it is often difficult to get the patients early enough’ (Medical Superintendent’s Annual Report, 1948). Many case notes attest to patients becoming more manageable after a course of ICT, yet many returned to their original state after only a few months, demonstrating that yet again the doctors had been too enthusiastic about its benefits. The treatment did, however, bring psychiatry closer to general medicine. Insulin was by then accepted as a pharmaceutical agent and the British legislation demanded that the treatment be given in a specially designed unit, similar to the units in general hospitals. This regulation put the DCMH under great strain. Running at full capacity and with no view of spatial expansion, the establishment of such treatment units on both male and female sides took two years (Medical Superintendent’s Annual Report, 1948). ICT was carried out as often possible, but correspondence suggests that there were waiting lists for patients for vacancies in the Insulin Ward. While the Medical Superintendent seemed pleased to report successful treatment to the relatives, he remained cautious about long-term prospects, and continuing correspondence suggests frequent relapses of patients. Insulin treatment was also praised by the Visiting committee (Visitors’ Handbooks, 1948 & 1949).
The extent of spatial constraints and their impact on the provision of treatments in the DCMH can be gleaned from the fact that the male Insulin Ward soon had to share its function with a third upcoming shock treatment – Electro-Convulsive Therapy (ECT) and that it was hoped to further subdivide this ward to make the treatment available to female patients as well (Visitors’ Handbook, 1948). Inducing shock by passing electricity through the patient’s body was first used in the DCMH in 1943 (Interview with Dr Jack). It had been developed in 1938 by Ugo Cerletti and Lucio Bini and before being introduced to the DCMH had been trialled at the Burden Neurological Unit in Bristol. This form of shock treatment was considered to be much safer than ICT or Cardiazol shock ( Fleming, Golla & Walter, 1939) and also much more cost-effective. Minimal staff training was required before the treatment could be given to a large number of patients within a short time period. In fact, in Devon it was frequently given at out-patient appointments from the 1950s onwards. Relaxants minimised the risk of bone fractures common to Cardizol shock and instant loss of consciousness reduced anxiety in patients. The DCMH experienced some trouble with the ECT apparatus in the beginning, resulting in bone fractures for several patients, but first results were nevertheless deemed promising. ECT did not have the same effect in all patients. While some relatives noted a significant change in the patient after only a few treatments, other patients experienced some initial relief, but fell back into their previous condition again – in which case many relatives asked for the continuation of the treatment. This confirms that relatives were getting increasingly involved in patients’ treatments, not only their admission and discharge. Despite some obvious success, the Medical Superintendent was reluctant to make statements regarding a patient’s future prospects.
Consent for ECT was again sought from patients’ relatives – even in the case of voluntary patients. In contrast to any other treatments trialled before, ECT seems to have been the first one to have raised concerns amongst relatives – or at least the first time they expressed such issues in letters to the Medical Superintendent. One lady, for example, who had agreed to ECT and later received a letter saying that her husband had fractured ‘three bones in the vertebrae column’ responded with the following letter ‘[…] That is the reason why it took me so long to sign the consent form as I feared that this might happen, but did not want to affect his recovery by not signing and did so’ (Correspondence regarding ED). She was particularly concerned about any long-term consequences. It is remarkable how many relatives agreed to treatments they were completely ignorant of, as this correspondence reveals: ‘Thank you for your intimation that [our son] is starting a course of Electrical Convulsive Treatment – needless to say I do not know what all that means, but I do know you will apply same for his help and benefit’. Others, as this lady’s letter illustrates, consented to treatment they knew the patient might be hesitant to agree to: ‘I am quite agreeable to whatever you think best […] I leave my husband in your hands knowing that you will do the best of your ability but I am afraid that you might have to persuade my husband because he seemed worried over the electrical treatment […]’. Trust in the Medical Superintendent seems to have outweighed any concerns. In other cases relatives consented to the treatment for the second time after the patient tried it and refused to continue, and the hospital seemed to rely on relatives to persuade the patient. These letters also show how much hope relatives placed in the treatment. In most cases patients ended up having the treatment, but it is not discernible what caused the change of mind. For the first time case notes give evidence that several (voluntary) patients refused either to have ECT at all or accepted to have one or two treatments, but refused further.
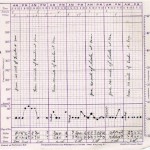
ECT had originally been introduced for people suffering from schizophrenia, but in the DCMH the benefits to patients suffering from depression or manic-depression became evident. On these grounds, patient 254 was the recipient of ECT on various admissions starting in 1949. One course of ECT consisted of 8 treatments, usually given at alternating days and recorded on special ECT charts. The treatment had a calming effect on patient 254 and reduced her hospitalisation considerably. The use of ECT declined with the advent of drug treatment, but interestingly, the late 1960s witnessed a resurgence of ECT – possibly because the limitations of the drugs had been recognised by then and more detailed research allowed for better evaluation of its efficacy. ECT is the only shock treatment that survived until the present day, although for a much smaller number of patients selected according to strict criteria, mainly patients who fail to respond to other forms of treatment. Contrary to other shock treatments, meta-analyses of ECT trials compared to psychopharmacological treatment have proved its efficacy (Janicak, Davis, Preskorn & Aydy, 1997).